J immunol:肿瘤免疫检查点疗法联合药物研究新进展
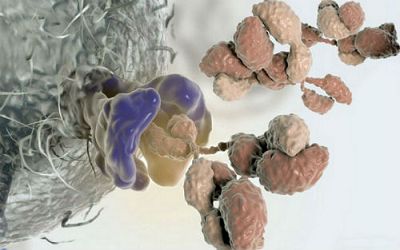
(图片摘自www.sciencealert.com)
癌症免疫疗法对特定类型的癌症具有显著的治疗效果,但单一的免疫治疗策略往往治疗效果有限,因此,在实践中往往需要结合两种或多种免疫治疗手段进行癌细胞的杀伤。
Anti-CD40抗体是天然免疫与后天免疫的激活剂之一,它能够有效激活癌症患者中的抗肿瘤免疫反应。临床上该药物也能够延缓胰腺癌患者的发病时间。此外,小鼠水平的试验也表明抗CD40抗体能够有效激活巨噬细胞,而且在天然免疫刺激的共同作用下还能够有效延缓特定癌细胞的生长。
众所周知,CTLA-4与PD-1是最常见的免疫检查点疗法的靶点分子,特异性针对CTLA-4与PD-1的抗体能够有效促进T细胞的激活,并对癌细胞进行杀伤。
在此基础上,来自美国威斯康星州立大学麦迪逊分校的Paul M. Sondel课题组研究了CD40与已有的免疫检查点药物联合使用的条件下对肿瘤特异免疫反应的诱导作用。相关结果发表在最近一期的《Journal of immunology》杂志上。
此前研究已经表明。系统性的对患有肿瘤的小鼠注射抗CD40抗体以及CpG能够有效刺激T细胞的激活,CTLA-4则能够进一步增强这一反应。在本研究中,作者发现肿瘤间隙注射CpG与anti-CD40抗体则能够有效抑制黑色素瘤的生长,但在T细胞缺失突变的小鼠模型中该效应也同时存在,这说明这一效应并不依赖于肿瘤特异性T细胞反应。事实上,作者发现具有抗肿瘤活性的细胞类型是巨噬细胞。
进一步,作者同时证明了CpG与anti-CD40注射引发的巨噬细胞活化后能够同时激活肿瘤特异性的T细胞反应。
之后,作者尝试了不同类型的免疫靶向药物的组合:包括IL-2与anti-CTLA-4的组合,anti-CD40/CpG与anti-CTLA-4的组合。结果显示,这些药物组合能够更好地引起抗肿瘤免疫反应,而抗肿瘤特异性T细胞也参与了这一过程。
最后,作者证明了这些药物联合刺激能够产生较长时间的免疫记忆(长达2-7个月)。
综上,这一研究揭示了anti-CD40与免疫检查点疗法药物联合使用能够更好地起到抗肿瘤免疫反应。(生物谷Bioon.com)
doi: 10.4049/jimmunol.1601073
PMC:
PMID:

doi: 10.4049/jimmunol.1601255
Effective Combination of Innate and Adaptive Immunotherapeutic approaches in a Mouse Melanoma Model
Alexander L. Rakhmilevich, Mildred Felder, Lauren Lever, Jacob Slowinski, Kayla Rasmussen, Anna Hoefges, Tyler J. Van De Voort, Hans Loibner, Alan J. Korman, Stephen D. Gillies and Paul M. Sondel
Most cancer immunotherapies include activation of either innate or adaptive immune responses. We hypothesized that the combined activation of both innate and adaptive immunity will result in better antitumor efficacy. We have previously shown the synergy of an agonistic anti-CD40 mAb (anti-CD40) and CpG-oligodeoxynucleotides in activating macrophages to induce tumor cell killing in mice. Separately, we have shown that a direct intratumoral injection of immunocytokine (IC), an anti-GD2 Ab linked to IL-2, can activate T and NK cells resulting in antitumor effects. We hypothesized that activation of macrophages with anti-CD40/CpG, and NK cells with IC, would cause innate tumor destruction, leading to increased presentation of tumor Ags and adaptive T cell activation; the latter could be further augmented by anti-CTLA-4 Ab to achieve tumor eradication and immunological memory. Using the mouse GD2+ B78 melanoma model, we show that anti-CD40/CpG treatment led to upregulation of T cell activation markers in draining lymph nodes. Anti-CD40/CpG + IC/anti-CTLA-4 synergistically induced regression of advanced s.c. tumors, resulting in cure of some mice and development of immunological memory against B78 and wild type B16 tumors. Although the antitumor effect of anti-CD40/CpG did not require T cells, the antitumor effect of IC/anti-CTLA-4 was dependent on T cells. The combined treatment with anti-CD40/CpG + IC/anti-CTLA-4 reduced T regulatory cells in the tumors and was effective against distant solid tumors and lung metastases. We suggest that a combination of anti-CD40/CpG and IC/anti-CTLA-4 should be developed for clinical testing as a potentially effective novel immunotherapy strategy.